How often to pediatricians perform a separate and identifiable E&M service during a well visit? I have some interesting information for those who are interested. The topic of the use of -25 modifiers, however, frustrates me considerably. I'm frustrated for two reasons.
First, the payors have been using the -25 modifer as a method for denying payment to pediatricians for years. My reasoning? Tell me, what is the difference from a clinical or narrative or service perspective between these two visits:
99393 (well visit)
90460 (imms admin)
90651 (HPV vaccine)
vs.
99393-25 (well visit...now with a -25 modifier)
90460 (imms admin)
90651 (HPV)
There is no difference. None. Zero. The same thing happened in both visits. Oh, wait, there is a difference - a bunch of payors, especially the usual suspect national ones, require that -25 modifier in order to be paid because...why? Given that the -25 modifier there adds no additional information (it makes the data worse, actually, as I point out below), given that there's no clinical benefit, given that there is no analytical benefit, I'm left to conclude that the only reason the payors inconsistently require a -25 modifier is to occasionally deny payment. Please, someone explain to me how I'm wrong.
The second reason I'm frustrated is that, as a result of this bogus coding requirement, many pediatric practices tend to slap -25 modifiers on everything under the sun. Well visits, sick visits, imms admin codes, screening tools, you name it. As a result, it's impossible to actually to any analysis of a practice's work using just CPT codes. You can't simply count up all the sick visits looking for -25s and determine the number visits that rose to both levels of service. It creates really messy gross data.
I've been meaning to do this for a while, but with the help of the PedSol team here at PCC, we looked through a few million appointments over the last 18m. Here's what the distribution looks like:
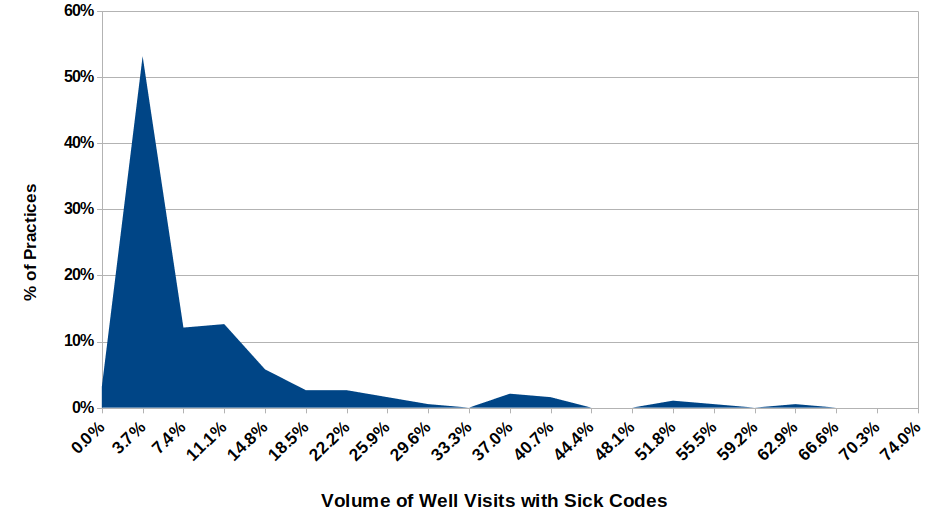
How to read this graph? About 55% of our clients billed about 5% of their well visits with an additional sick visit. You'll notice the long tail - that's right. There are practices who are billing as many as 45% or 55% or even more than 70% of their well visits with an additional sick code. But they are not common.
The bottom line is that our clients code a sick visit during a well visit 5.7% of the time.
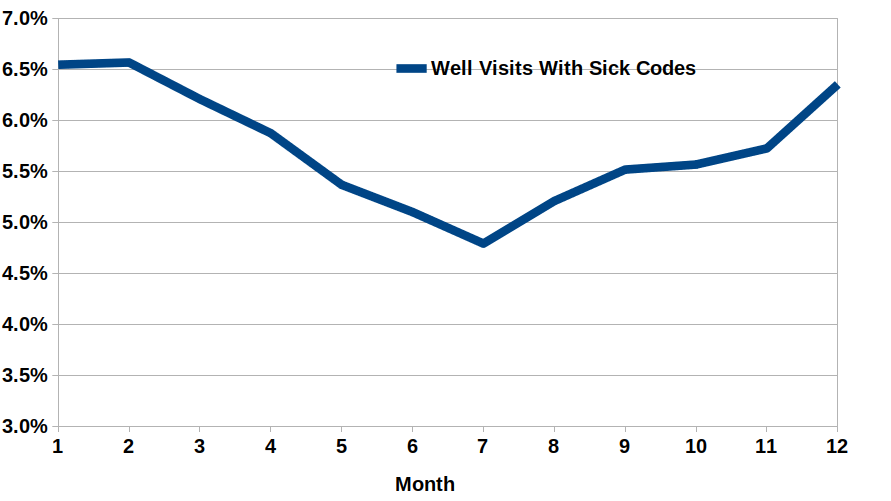
What I also found interesting is the cycle of volume that exists. We shouldn't be surprised to learn, I think, to see that sick visits are much more common in the winter time, when kids are often sickest. But there it is.
Comments, insight welcomed.
Comments
6 Comments